Patient Eligibility & Triggers
for Hospice Care
Palmetto GBA Local Coverage Determination

Overview
Prevent High-Risk Hospital Readmissions
Hospice care is a valuable resource for healthcare workers seeking to prevent high-risk hospital readmissions. It is essential to help healthcare workers understand the special eligibility requirements needed when considering hospice services, such as age, diagnosis, and prognosis criteria.
Healthcare professionals can reduce the burden on medical facilities by ensuring patients are eligible for hospice care.
Let HOPE Add Life To Your Days
HOPE Healthcare and Hospice was created by a local and experienced group of healthcare professionals passionate about making a difference in the lives of those touched by advanced illness.
We proudly serve nine parishes in Acadiana, including Acadia, Evangeline, Iberia, Jefferson Davis, Lafayette, St. Landry, St. Martin, St. Mary, and Vermilion.
General Eligibility
Determining a primary hospice diagnosis can be challenging when a patient has some, but not all, of the clinical indicators of a specific disease or condition.
The following clinical signs often support hospice eligibility in combination with another primary diagnosis.
- Rapid decline over the past three to six months, evidenced by:
- Rapid progression of the disease
- Progressive decline in Palliative Performance Score (PPS)*
- Weight loss not due to reversible causes and/or declining serum albumin levels
- Dependence on assistance for two or more ADLs:
- feeding, ambulation, continence, transfer, bathing, or dressing
- Dysphagia leading to inadequate nutritional intake or recurrent aspiration.
- Decline in systolic blood pressure to below 90 systolic or progressive postural hypotension.
- Increasing ER visits, hospitalizations, or physician follow-up
- Multiple progressive Stage 3 or Stage 4 pressure ulcers despite optimal care
- Frequent falls or increasing problems with balance and weakness.
- Increased lethargy/sleepiness
- Uncontrolled pain, shortness of breath, nausea/vomiting, anxiety
- Multiple, recurrent infections
- Patient appears to be “giving up” physically and emotionally.
HOPE Healthcare and Hospice is available 24/7 to assist in identifying whether a patient may be eligible for hospice services.
Amyotrophic Lateral Sclerosis (ALS)
Patients will be considered to be in the terminal stage of ALS (life expectancy of six months or less) if they meet the following criteria.
- Patients should demonstrate critically impaired breathing capacity.
- Dysphasia
- Wheelchair or bed-bound status
- Needs assistance in most or all (ADLs)
Alzheimer's Disease
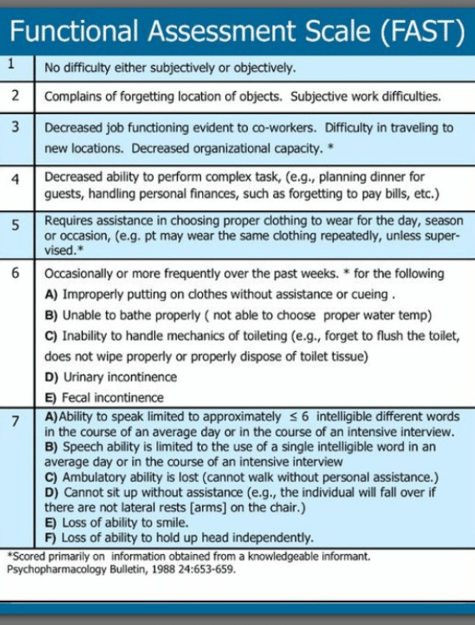
The FAST scale is a 16-item scale designed to parallel the progressive activity limitations associated with AD. Stage 7 identifies the threshold of activity limitation that would support a 6-month prognosis.
Stage 7: Loss of speech, locomotion, and consciousness:
7a: Ability to speak limited (1 to 5 words a day)
7b: All intelligible vocabulary lost.
7c: Non-ambulatory
7d: Unable to sit up independently.
7e: Unable to smile.
7f: Unable to hold head up.
The FAST scale does not address the impact of comorbid and secondary conditions.
Secondary conditions that are often related to and/or complicate Alzheimer's:
- Recent Falls
- UTI's
- Infections
- Pressure Ulcers
- Weight Loss
- Delirium
Structural/functional impairments and relevant activity limitations:
- Ambulation
- Continence
- Transfer
- Dressing
- Eating
- Bathing
Cancer
Medicare requires "clinical information and other documentation" to support the certification of individuals having a terminal illness with a life expectancy of 6 months or less if the disease runs its normal course.
There are many types of cancer; the following hospice cancer criteria are general rules physicians can use to determine if hospice is the right choice for a patient.
Clinical hospice cancer criteria may include the following:
- Metastatic cancer
- Decline in the condition despite therapy
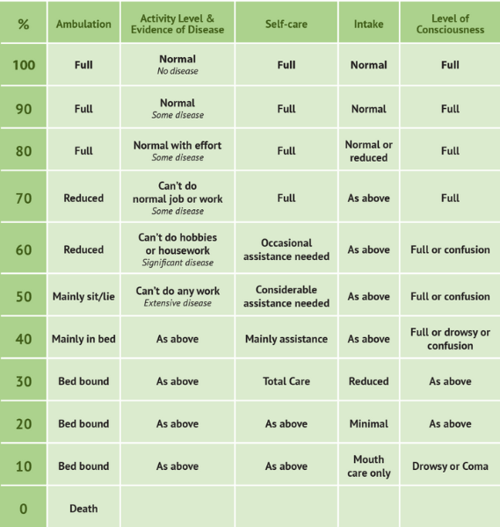
- Palliative Performance Score of 70% or less
- Electing to forgo further disease-directed curative treatment. (Palliative radiation or chemotherapy may still be included.)
Specific cancer diagnoses are often eligible for hospice without other criteria, including small cell lung cancer, pancreatic cancer, and primary CNS malignancy.
The Palliative Performance Scale is used to assess the progressive decline of palliative patients and is frequently used to determine if a cancer patient is eligible for hospice.
Cardiac/Heart Disease
Medicare requires "clinical information and other documentation" to support the certification of individuals having a terminal illness with a life expectancy of 6 months or less if the disease runs its normal course.
The International Classification of Functioning includes the following domains (Ranking No, Mild, Moderate, Severe, Complete Impairment):
- Structures of Cardiovascular & Respiratory Systems
- Functions of Cardiovascular & Respiratory Systems
- Communication
- Mobility
- Self-care
Identification of specific structural/ functional impairments and relevant activity limitations:
- Heart Valve Stenosis
- Ambulation
- Class IV NYHA
- Incontinence
- Difficulty with Transfers
- Severely reduced Ejection Fraction
- Impaired Self-care
- Abnormal Lab Values
- Abnormal oxygen saturation
- Irregular lung sounds
These impairments contribute to the increased incidence of secondary conditions, such as:
- Delirium
- Pneumonia
- Stasis Ulcers
- Pressure ulcers
- Falls
- Weight Loss
- Oxygen Dependence
- Other Infections
SPECIFIC DATA TO SUPPORT A HOSPICE DIAGNOSIS OF CHF:
- Identification of specific structural/functional impairments
- Ejection fraction <20% (not required, but an important consideration)
- A poor response to diuretics and vasodilators
- Dyspnea or tightness in the chest despite tx.
- Chest pain
- Impaired heart rhythms, contraction force of ventricular muscles, and impaired blood supply to the heart
- Changes in appetite, unintentional weight loss
- Impaired sleep functions
- Decline in general physical endurance
- Relevant activity limitations and or impaired mobility
If you are seeing any of the above signs and symptoms in a patient with CHF or end-stage cardiac conditions, it may be time to consider adding the support of hospice care.
SPECIFIC DATA TO SUPPORT A HOSPICE DIAGNOSIS OF COPD:
- Recent visits to the ER or hospitalization for pulmonary infections or respiratory failure
- Dyspnea or tightness in the chest (FEV1 <30% of predicted)
- Identification of specific structural/functional impairments
- Relevant activity limitations
- Changes in appetite and unintentional progressive weight loss
- Impaired sleep functions
- Decline in general physical endurance
- Impaired mobility
- Requires oxygen most, if not all, of the time
- May require breathing treatments or the use of inhalers
- May have difficulty eating or carrying on conversations without becoming short of breath.
End-Stage Renal Disease
End-stage renal disease (ESRD) may support a prognosis of six months or less under many clinical scenarios.
Documenting structural/functional impairments and activity limitations facilitates the selection of intervention strategies (palliative vs. long-term disease management/curative). It provides objective criteria for determining the effects of such interventions.
- Creatinine clearance of <10cc/min (<15cc/min for diabetics) AND serum creatinine >8.0 mg/di (>6.0mg/di for diabetics)
- Uremia with obtundation
- Nausea/Vomiting
- Patient has chosen not to have renal dialysis
- Intractable hyperkalemia
- Hepatorenal syndrome
- Structural and functional impairments
- Platelet count <25,000
- Comorbid and secondary conditions contribute to terminal prognosis
- Pruritus
- Self-care deficits
- Activity limitations
- Uremic pericarditis
- Anorexia
- Albumin < 2.5 gm/di
General Debility
General Debility is characterized by unexplained weight loss, malnutrition, and disability. The Two defining clinical elements are:
- Nutritional impairment
- Disability
The nutritional impairment and disability associated with the general debility may be severe enough to impact the patient's short-term survival.
- The nutritional impairment associated with the general debility should be severe enough to impact a beneficiary's weight. It is expected that the Body Mass Index (BMI) for an adult FTT syndrome patient will be below 22 kg/m2 and that the patient is either declining enteral/parenteral nutritional support or has not responded to such nutritional support, despite an adequate caloric intake.
- The disability associated with the adult FTT syndrome should be such that the individual is significantly disabled. Significant disability would be demonstrated by a Karnofsky or Palliative Performance Scale value less than or equal to 40%.
Note: If an individual does not meet the medical criteria listed above but is still thought to be eligible for Hospice, an alternate diagnosis that best describes the clinical circumstances of the individual should be selected.
The following must be documented:
- A current BMI is calculated with the beneficiary’s height and weight.
- A current evaluation of the patient's functional status demonstrating a disability equivalent to that described by a KPS or PPS value of less than or equal to 40% is determined.
- Within six months (180 days) of the most recent certification/recertification date for beneficiaries without enteral nutritional support.
OR,
- At the time of initial certification and during each subsequent recertification for beneficiaries receiving enteral nutritional support, Abnormal weight loss, and cachexia are additional secondary diagnoses that may describe the clinical circumstances.
Note: Adult Failure to Thrive and Debility cannot be used as the primary hospice diagnosis.
HIV/AIDS
Human Immunodeficiency Virus (HIV) Disease (1 and 2 must be present; factors from 3 will add supporting documentation)
1. CD4 + Count 100,000 copies/ml, plus 1 of the following:
- CNS lymphoma
- Untreated or not responsive to treatment, wasting (loss of 33% lean body mass)
- Mycobacterium avium complex (MAC) bacteremia, untreated, unresponsive to, or refused treatment.
- Progressive multifocal leukoencephalopathy
- Systemic lymphoma, with advanced HIV disease and partial response to chemotherapy
- Visceral Kaposi's sarcoma & unresponsive to therapy
- Renal failure in the absence of dialysis
- Cryptosporidium infection
- Toxoplasmosis, unresponsive to therapy
2. Decreased performance status as measured by the Palliative Performance Scale (PPS).
3. Documentation of the following factors will support eligibility for hospice care:
- Chronic persistent diarrhea for one year
- Persistent serum albumin < 2.5
- Concomitant, active substance abuse
- Age > 50 years
- Absence of antiretroviral, chemotherapeutic, and prophylactic drug therapy related specifically to HIV disease.
- Advanced AIDS dementia complex
- Toxoplasmosis
- CHF symptomatic at rest
Hospice Non-Cancer Diagnosis
Medicare coverage of hospice care depends upon a physician's certification of a patient's prognosis of a life expectancy of 6 months or less if the terminal illness runs its normal course. Some patients may not meet these criteria yet still be appropriate for hospice care because of other comorbidities or rapid decline. Coverage for these patients may be approved on an individual consideration basis.
Documentation requirements are as follows:
- Documentation supporting the medical necessity should be legible and maintained in the patient's medical record.
- Documentation certifying terminal status must contain enough information to confirm terminal status upon review.
- If the patient does not meet the criteria outlined under the Coverage Indication Section of this book yet is deemed appropriate for hospice care, sufficient documentation of the patient's condition that justifies terminal status in the absence of meeting the criteria would be necessary.
Liver Disease
Patients will be considered to be in the terminal stage of liver disease if they meet the following criteria (1 and 2 must be present factors from 3 will lend supporting documentation):
- The patient should show both a and b:
- Prothrombin time prolonged more than 5 seconds over control or International Normalized Ratio (INR) > 1.5
- Serum albumin < 2.5 gm/di
- End-stage liver disease is present, and the patient shows at least one of the following:
- Ascites, refractory to treatment, or patient noncompliance
- Spontaneous bacterial peritonitis
- Hepatorenal syndrome (elevated creatinine and blood urea nitrogen (BUN) with oliguria (<400 ml/day) urine sodium concentration <10 mEq/I)
- Hepatic encephalopathy, refractory to treatment, or patient non-compliance
- Recurrent variceal bleeding despite intensive therapy
- Documentation of the following factors will support eligibility for hospice care:
- Progressive malnutrition
- Muscle wasting with reduced strength and endurance
- Continued active alcoholism (> 80 gm ethanol/day)
- Hepatocellular carcinoma
- Hepatitis B virus surface antigen (HBsAg) positivity
- Hepatitis C is refractory to interferon treatment.
- Patients awaiting liver transplants who otherwise fit the above
Criteria may be certified for the Medicare hospice benefit, but the patient must be discharged from hospice if a donor organ is procured.
SPECIFIC DATA TO SUPPORT HOSPICE DIAGNOSIS OF LIVER DISEASE
- Weakness and compromised ability to perform activities of daily living (ADLs)
- Recurrent variceal hemorrhage
- Hepatic encephalopathy
- Prothrombin time prolonged more than five seconds over control or INR > 1.5
- Serum Albumin < 2.5 gm/di
- Peritonitis
- Elevated creatinine and BUN with Oliguria <400 ml/day and urine Na concentration <10 mEq/I
- Ascites
- Malnutrition
- Muscle wasting
- Asterixis
- May be awaiting a liver transplant but would be discharged if a donor is procured.
Neurological Conditions (Non-Alzheimer's)
The information below is a guideline to support the prognosis of six months or less and will lend supporting documentation to help define coverage.
This LCD presents a framework for identifying, documenting, and communicating the unique healthcare needs of individuals with neurological conditions.
Neurological conditions are associated with impairments and disability. Their impact on any individual depends on their overall health status.
For neurological conditions, secondary conditions could include:
- Dysphagia
- Pneumonia
- Pressure ulcers
The following components should be addressed in your documentation:
- Structures of the nervous system
- Mental function
- Sensory functions and pain
- Neuromusculoskeletal and movement functions
- Communication
- Mobility issues
- Self-care ability
While every category may not apply to every individual with a neurological condition, these categories represent a set of body functions, body structures, activities, participation, and environmental factors that could inform decision-making for patients with neurological conditions at the end of life.
SPECIFIC DATA TO SUPPORT A HOSPICE DIAGNOSIS OF A NEUROLOGICAL DISORDER:
- Structural/functional impairments
- Impaired mental function
- Impaired sensory function and pain
- Impaired neuromusculoskeletal and movement functions
- Impaired communication
- Impaired mobility
- Self-care deficit
- Activity limitations
Comorbid and secondary conditions also contribute to a terminal prognosis.
SPECIFIC DATA TO SUPPORT A HOSPICE DIAGNOSIS OF A CVA:
- Palliative Performance Score or Karnofsky Score of 40% or less.
- Mainly bed-to-chair bound.
- Impaired functional status
- Requires assistance with activities of daily life (ADLs)
- Changes in orientation status
- Unable to maintain sufficient fluid and caloric intake.
- Progressive weight loss
- Dysphagia
Stroke
Regardless of the specific diagnosis, patients with neurological diseases are eligible for hospice services when they experience a continuous decline in functional or clinical status over time, leading to a poor prognosis with a life expectancy of six months or less if they meet the following criteria:
- Karnofsky Performance Status (KPS) or Palliative Performance Scale (PPS)
of 40% or less - Inability to maintain hydration and caloric intake with one of the following:
- Weight loss > 10% in the last six months or > 7.5% in the last three months
- Serum albumin < 2.5 gm/dl
- Current history of pulmonary aspiration
- Not responsive to speech-language pathology intervention
- Sequential calorie counts documenting inadequate caloric/fluid intake.
- Dysphagia severe enough to prevent the patient from receiving food and fluids necessary to sustain life in a patient who declines or does not receive artificial nutrition and hydration.
Coma (Any Etiology)
Regardless of the specific diagnosis, patients with neurological diseases are eligible for hospice services when they experience a continuous decline in functional or clinical status over time, leading to a poor prognosis with a life expectancy of six months or less if they meet the following criteria:
Comatose patients with any 3 of the following on day three of coma:
- Abnormal brain stem response
- Absent verbal response
- Absent withdrawal response to pain
- Serum creatinine > 1.5 mg/dl
Specific Data to Support a Hospice Diagnosis of Dementia
For dementia patients to meet the hospice eligibility criteria, they must have a life expectancy of six months or less if the disease continues in its typical progression. The patient's dementia type must be specified, i.e., Alzheimer's Disease, Parkinson's, Lewy Body. It may be time to consider hospice when their physical condition declines. Some key things to look for include the following:
- A diagnosis of conditions such as COPD, CHF, cancer, or congenital heart disease
- An increase in hospitalizations, frequent visits to the doctor, and/or to the ER
- A diagnosis of pneumonia or sepsis
- Weight loss or dehydration due to challenges in eating/drinking
- Speech limited to six words or less per day.
- Difficulty swallowing or choking on liquids or food.
- Urinary and fecal incontinence
- Unable to sit upright without armrests on chairs or may slip out of chairs and require sitting in special chairs.
- Unable to walk without the assistance of a person or device.
- Unable to sit up without assistance (will slump over if not supported)
- No longer able to smile.
General Guidelines for Eligibility
The following may be applied to patients who do not fall under any disease-specific guidelines.
Documented clinical progression of the disease may include:
- The progression of a disease process as listed in disease-specific criteria, as documented by practitioners' assessment and/or lab, radiologic, or other studies.
- Multiple emergency department or inpatient hospitalizations over the prior six months.
- Home health nursing assessment if the patient has been receiving home health services.
- AND/OR Recent decline in functional status may be documented. The functional decline should be recent to distinguish terminal patients from those with reduced baseline functional status due to chronic illness. Either may document diminished functional status:
- Palliative Performance Scale value of <30
- Dependence in at least 3 of 6 ADLs:
- Bathing, dressing, feeding, transfers, continence of urine or stool, ability to ambulate independently to bathroom and/or
- Recent impaired nutritional status:
- Unintentional progressive weight loss of >10% in six month
- Serum albumin less than 2.5 gm/dl may be used as a prognostic indicator, but not in isolation from the factors above.
New York Heart Association (NYHA) Classification of Severity Heart Failure
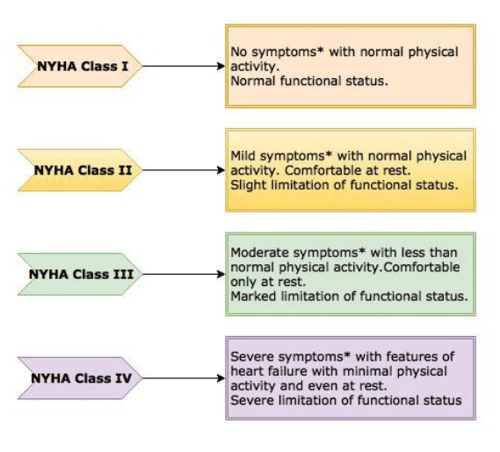
| Class I (mild) | No limitation on physical activity. Ordinary physical activity does not cause undue fatigue, palpitation, or dyspnea (shortness of breath) |
| Class II (mild) | Slight limitation of physical activity. Comfortable at rest, but ordinary physical activity results in fatigue, palpitation, or dyspnoea |
| Class III (moderate) | Marked limitation of physical activity. Comfortable at rest, but less than ordinary activity causes fatigue, palpitation, or dyspnoea |
| Class IV (severe) | Unable to carry out any physical activity without discomfort. Symptoms of cardiac insufficiency at rest. If any physical activity is undertaken, discomfort is increased |
Resources
For more information on best clinical practices, documentation, regulations, and operations, here are some helpful websites: